Genetics of Cancer - I
Introduction:
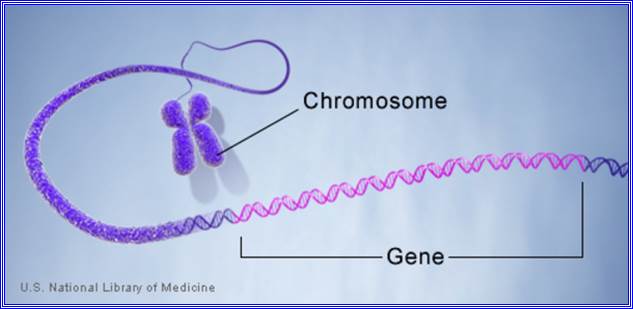
Organisms are made up of tissues and tissues are made up of cells, which are fundamental structural and molecular functional units of organ structure and function.� The number of cells per organisms vary from single cell to more than 1018 cells, where one finds different cell types, for example human body consists of approximately 10^14 cells and more than 210-320 (?) different cell types.� During growth and development there is a continuous addition of cells that is responsible for the growth in size and development of an organism.� When grown to a size, some cells die and they are immediately replaced; thus cell replacement balance the cell death thus maintain the tissue size.� However circulating cell types are also subjected to turn over, but their population sometimes varies depending upon certain situations, but in normal situations the cell number is maintained, that includes cell division of their kind and death of their kind, finally the cell population of each kind is maintained.
In human body the most abused tissue cells are oral and intestine epithelial cells, and have the half-life of few days and they are rapidly replaced.� RBC cells are replaced once in 120 days, liver cells hardly die ���(normally they are replaced) and brain cells die with age without any replacement.�� Each cell in a tissue performs its own specified function or functions.� It is remarkable that all kinds of cells have the same amount of genome, but the type of the genes and the number of genes and the level of each gene expressed in each tissue and cell type is different; that is the marvel of life; that is the difference between life and nonliving materials; but it is a fact that life is made up of non-living innate matter, but in dynamic combinations, which can make it living or nonliving.� Regulation of gene activity in each of the cells is strictly regulated, but occasionally activity of some genes go out of control because of mutations, that leads the abnormal behavior of cells, which can lead to disease, cell death, or uncontrolled multiplication of cells into cancer.
����������������������������������������������� ������� 
�������������������������������������������������� 
����������� XY chromosomes
������������� ������������� 
��������� ������ X chromosome
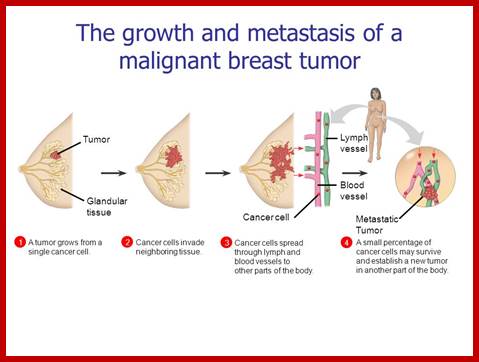
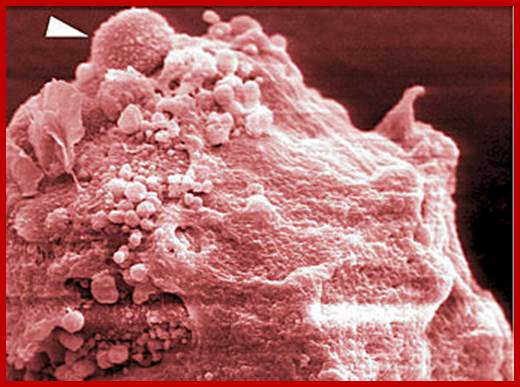
Cells, which have acquired the ability to live, divide and redivide and spread forever in undifferentiated mass of cells, are called cancer cells. He La cells are cancer cells, from Henrietta Lacks are maintained for many decades. Ascites cells can be grown in mice.� Cancer cells are the most dynamic and healthy cells, the only purpose of these cells is to proliferate and remain alive, and they have acquired such ability. Tumor, another name for a type of cancer, is mass of cells, which grow in number ceaselessly, without control.� These cells can proliferate; migrate to different areas of the body, but don�t differentiate into cell types.
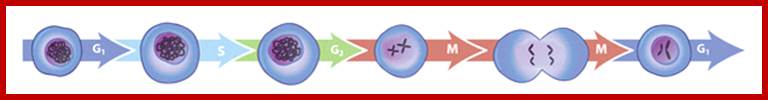
The sequence of eukaryotic cell cycle phases: Between each arrow, the cell passes through a particular cell cycle checkpoint. http://www.nature.com/
Proto-oncogene and Oncogene;
Proto-oncogenes normal cellular genes that promote cell growth in a variety of ways. Many can produce hormones, "chemical messengers" act on cells that encourage mitosis of cells, the effect of which depends on the signal transduction of the receiving tissue or cells. Some are responsible for the signal transduction system and signal receptors in cells and tissues themselves, thus controlling the sensitivity to such hormones. Some often produce mitogens, or some are involved in transcription of DNA in protein synthesis, which in turn produce the proteins and enzymes which are involved in producing various cellular biochemicals and cells use them. Any gene on mutation lead to wrong function, leads to cancer.
Proto-oncogenes are cellular genes code for proteins that help to regulate cell growth and differentiation. Proto-oncogenes are often involved in signal transduction and execution of mitogenic signals, usually through their protein products provided the certain mutations in the genome. Upon activation, a proto-oncogene (or its product) becomes a tumor-inducing agent, an oncogene. Examples of some proto-oncogenes include RAS, WNT, MYC, ERK, and TRK (wiki).
Mutations in proto-oncogenes can modify their expression and function, increasing the amount or activity of the product protein. When this happens, such genes become oncogenes.
Proto-oncogenes can become an oncogene by small but specific modifications.� This can be due to a mutation in its regulatory region ex. Promoter region. This can lead to increase in proteins and protein activity, and or loss of regulation.� Chromosomal translocation is also another possibility by translocation of the one gene to other position or translocation leading to fusion between proto-oncogene and a second gene.� Ex; Philadelphia chromosome is an example of this type of translocation from chromosome 22 and chromosome 9.
����������� ����������� 
https://www.linkedin.com/pulse
����������������������� ����������������������� http://www.lympomininfo.net
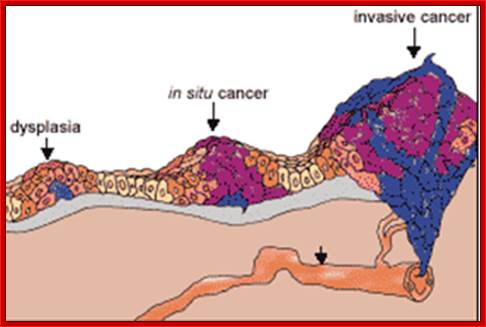
The figure depicts stages of cells go through before they become cancerous cells; http://www.cancer.ca/
Genetic tests; Genetic tests for breast, ovarian, colon, thyroid, and some other cancers, can tell whether a person from a family that shows signs of such a syndrome has one of these mutations. There are 50 or more tests available to detect cancer prone and benign cancer in a person; Lynch syndrome , Li-Fraumeni syndrome-gene 53, G PTENAPC gene, Retinoblastoma, BRCA1 and 2, Wermer syndrome, RET gene, VHL,� These tests can also show whether family members without obvious disease have inherited the same mutation as a family member who carries a cancer-associated mutation. (For more information, see this overview of genetic testing for hereditary cancer syndromes.).� Cancers that are not caused by inherited genetic mutations can sometimes appear to �run in families.�
Even if a cancer-predisposing mutation is present in a family, not everyone who inherits the mutation will necessarily develop cancer. Several factors influence the outcome in a given person with the mutation, including the pattern of inheritance of the cancer syndrome. More than 509 hereditary cancer have been identified.
Note- U.S. laboratories that perform health-related testing, including genetic testing, are regulated under the Clinical Laboratory Improvement Amendments (CLIA) program. Laboratories that are certified under CLIA are required to meet federal standards for quality, accuracy, and reliability of tests. All laboratories that do genetic testing and share results must be CLIA certified. However, CLIA certification only indicates that appropriate laboratory quality control standards are being followed; it does not guarantee that a genetic test being done by a laboratory is medically useful. Thus genetic test are regulated in USA.
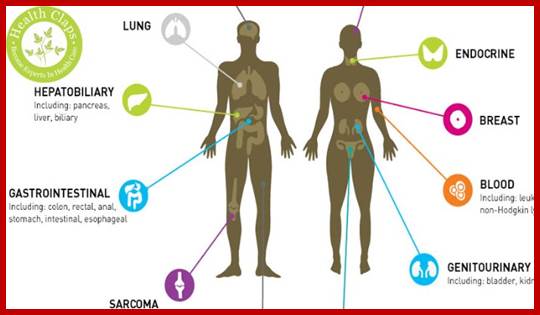
Cancers� categories:
Benign: are lumps.
Primary tumors: are solids.
Metastatic: are invasive.
List of cancer types and List of oncology-related terms;
Cancers are usually named using names such as -carcinoma, -Sarcoma or Blastoma as a suffix, with the Latin or Greek word for the organ or tissue of origin as the root. For example, a cancer of the liver is called hepatocarcinoma; a cancer of fat cells is called a liposarcoma. For some common cancers, the English organ name is used. For example, the most common type of breast cancer is called ductal carcinoma of the breast. Here, the adjective ductal refers to the appearance of the cancer under the microscope, which suggests that it has originated in the milk ducts.
http://www.medicinenet.com; �http://www.cancerresearchuk.org/; http://www.webmd.com/cancer/brain-cancer/
There are over 200 or more types of cancers; mutations in 291 genes implicated in oncogenesis far too numerous to include in this introductory article. Out of 25,000 human genome ensembles more than 1% of the genes are involved in cancer induction. Mutations in 291 genes have been implicated in oncogenesis, all encode proteins; no RNA genes are implicated, but some miRNAs are also involved has been observed.
Benign cancers: (which are not cancers) They are named using -oma as a suffix with the organ name as the root. For example, a benign tumor of smooth muscle cells is called a leiomyoma (the common name of this frequently occurring benign tumor in the uterus is fibroid). Confusingly, some types of cancer also use the -oma suffix, examples including melanoma and seminoma.
Cancer genes census:
Sorted by the type and the number; this is the list known as cancer genes (not complete and comprehensive).
|
Name |
No. |
|
Amplification |
15 |
|
Chromosome abnormal |
457 |
|
Frame shift mutation |
88 |
|
Germ line mutation |
75 |
|
Large deletion |
34 |
|
Missense mutation |
126 |
|
Nonsense Mutations |
85 |
|
Translocation |
315 |
|
Somatic mutations |
415 |
|
Splicing mutations |
53 |
|
Symbol |
457 |
|
Sn-mi RNA, Sno RNA and RISC |
135 -? |
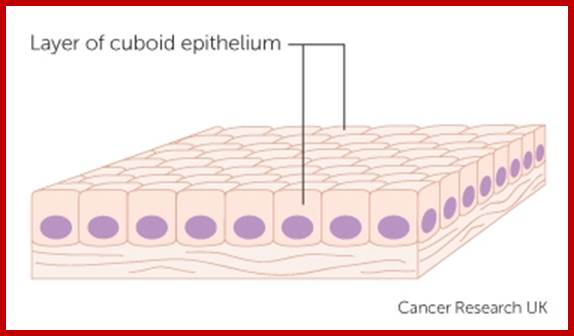
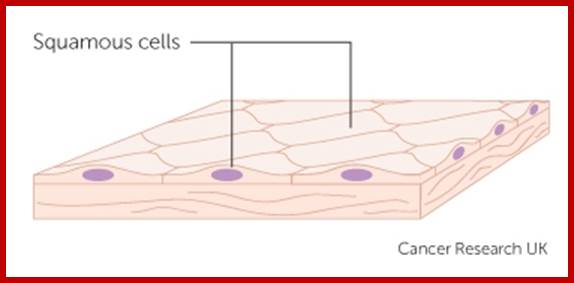
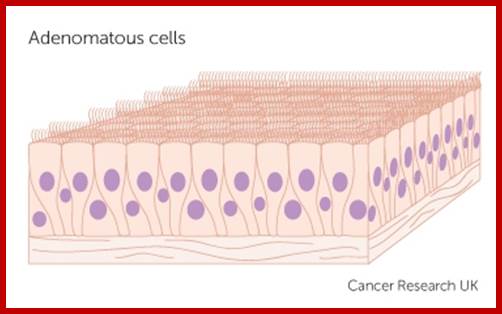
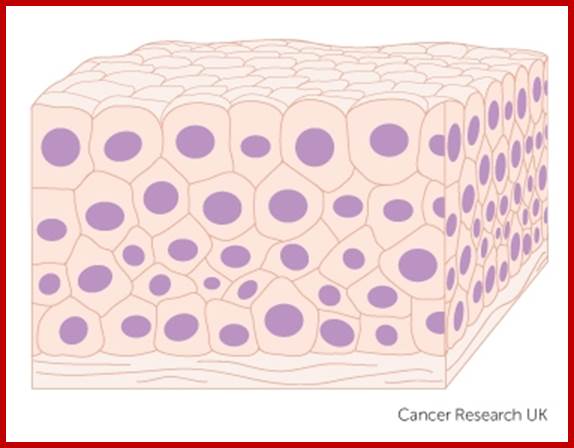
Carcinomas:
All those cancers develop from epithelia cells, epidermal and endodermal �surface layers are considered as Carcinoma; Types-
Ductal carcinoma in situ (DCIS)
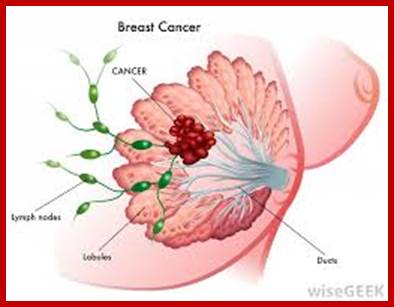
- Indications of Carcinomas- open sores, red patches, pink growths and shiny bumps or scars. Carcinoma: Cancer derived from epithelial cells. This group includes many of the most common cancers, including those of the breast, prostate, lung; This group includes many of the most common cancers, including those of the breast, prostate, lung and colon.
 �
�
http://www.cancerresearchuk.org/
http://www.cancerresearchuk.org/
http://www.cancerresearchuk.org/; http://www.medicinenet.com/: http://www.medicinenet.com :
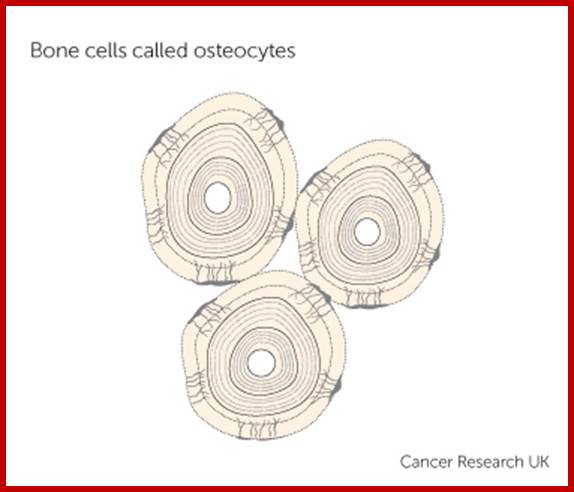
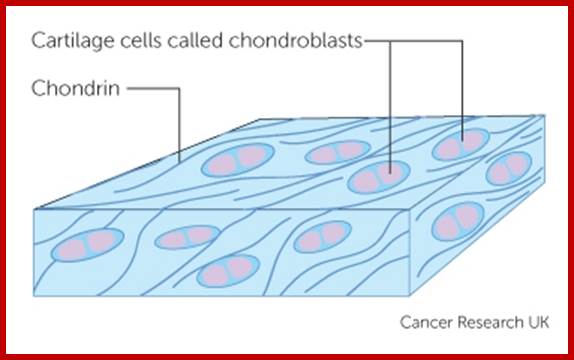
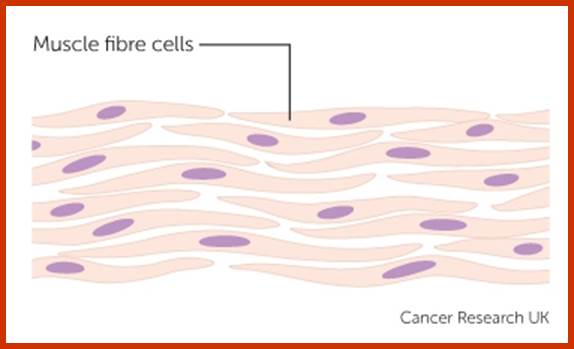
Sarcomas: All those cancers developed from mesoderm are called sarcomas.
Bone sarcoma; They develop from Bone cells. �Cancer that begins in bone, cartilage, fat, muscle, blood vessels, or other connective or supportive tissue � bone, soft tissue cancers," osteosarcoma, synovial sarcoma, liposarcoma, angiosarcoma, rhabdosarcoma, and fibrosarcoma osteosarcoma-"bone, soft tissue cancers, synovial sarcoma, liposarcoma, angiosarcoma, rhabdosarcoma, and fibrosarcoma; Sarcoma: Cancer derived from connective tissue, or mesenchymal cells.
http://www.cancerresearchuk.org/ Bone sarcoma
http://www.cancerresearchuk.org/
http://www.cancerresearchuk.org/
Soft tissue sarcoma: Develop from cartilage and muscle cells.
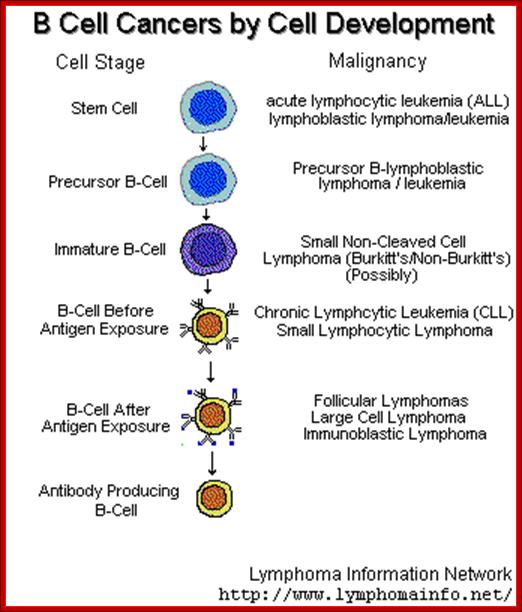
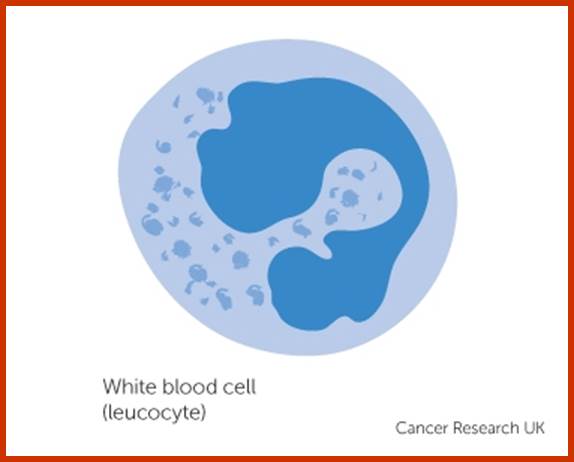
Leukemia: Blood cancers.
This, a group of cancers, that is grouped within blood cancers. These cancers affect the bone marrow which is the site for blood cell production. When cancerous, the bone marrow begins to produce excessive immature white blood cells that fail to perform their usual actions and the patient is often prone to infection
Types of leukemia include:
� Acute myelocytic leukemia (AML) � these are malignancy of the myeloid and granulocytic white blood cell series seen in childhood.
� Chronic myelocytic leukemia (CML) � this is seen in adulthood.
� Acute Lymphatic, lymphocytic, or lymphoblastic leukemia (ALL) � these are malignancy of the lymphoid and lymphocytic blood cell series seen in childhood and young adults.
� Chronic Lymphatic, lymphocytic, or lymphoblastic leukemia (CLL) � this is seen in the elderly.
� Polycythemia vera or erythremia � this is cancer of various blood cell products with a predominance of red blood cells.
http://www.cancerresearchuk.org/
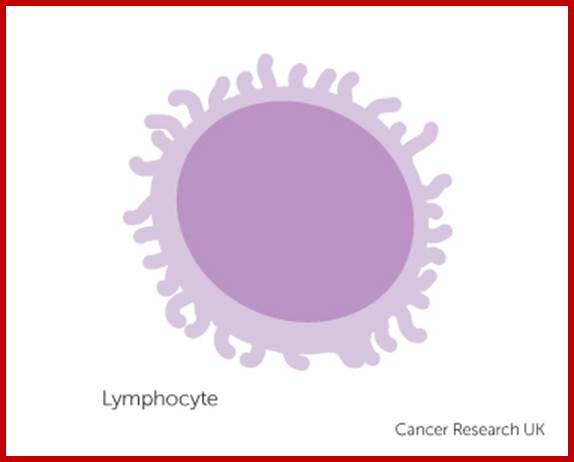
Lymphoma;
These are cancers of the lymphatic system. Unlike the leukemia, which affect the blood and are called �liquid cancers�, lymphomas are �solid cancers�. These may affect lymph nodes at specific sites like stomach, brain, intestines etc. These lymphomas are referred to as extra nodal lymphomas.
- Lymphomas may be of two types � Hodgkin�s lymphoma and non-Hodgkin�s lymphomas. They are considered as lymph system tubules and glands, lymph vessels and spleen. Such cells spread all over the body. Cancer derived from hematopoietic (blood-forming) cells, Cancers that begin in the cells of the immune system -- "lymphoma," T-cell lymphomas, B-cell lymphomas, Hodgkin lymphomas, non-Hodgkin lymphoma, and lymphoproliferative lymphomas
http://www.cancerresearchuk.org/
Myeloma: It is also known as multiple myelomas, they start from plasma cells like WBC in the bone marrow; they produce antibodies.� In myeloma cells become abnormal and multiply in large number, yet they produce only one type of antibodies.
Blastoma: Cancer derived from immature "precursor" or embryonic tissue. These are also commonest in children.
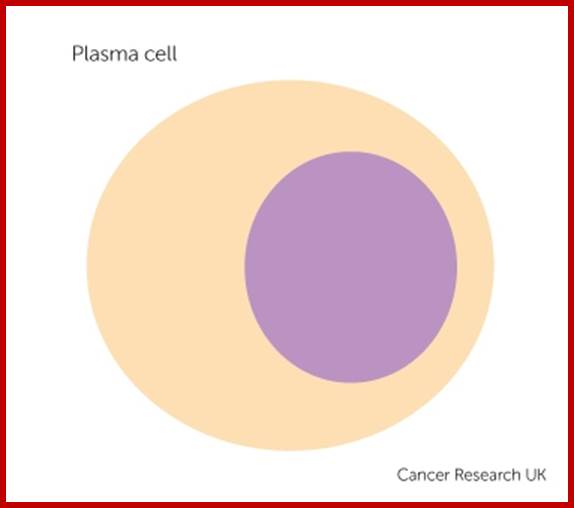
This cancer starts form plasma cells, which are a type of blood cells made in bones cells and bone marrow; http://www.cancerresearchuk.org/
Brain and spinal cord cancers: Malignant Gliomas, Metastatic Brain Tumors,
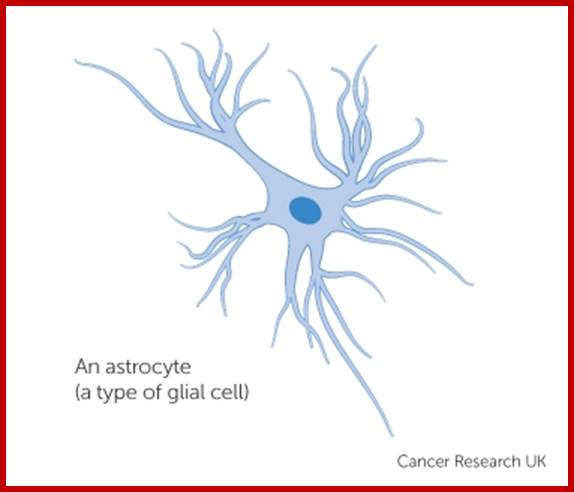
Brain and spinal cord tumours, they account 3 out of 100 cases of cancers.�� ��Central nervous system cancers: Cancers that begin in the tissues of the brain and spinal cord -- "brain and spinal cord tumors," gliomas, meningiomas, vestibular schwannomas, primary CNS lymphomas, and primitive neuroectodermal tumors. http://www.cancerresearchuk.org/; http://www.cancer.ca ttp://www.webmd.com/cancer/brain-cancer/
Cancers whatever may be the types; the cancer cells have lost regulated cell division. Once fully formed, ultimately invade every possible type of tissues in their neighborhood and cause damage entailing death of an organism, but cancer cells can also be taken out and cultured in vitro and maintained in the lab for any number years (ex. HELA cells). Any such cancers malfunctions, invade resulting in disabling an organism and cause death. So cancer can be called as genetic diseases for it stem from genetic disorder de-novo or such disorders can be vertically transmitted from tissue to the others.
Ten most important Cancers in USA:
|
Cancer site |
Cases per year |
Deaths per year |
|
Breast |
184,200 (15.1%) |
41,200 (7.5%) |
|
Prostate |
180,400 (14.8%) |
31,900 (5.8%) |
|
Lung |
164,100 (13.4%) |
156,900 (28.4%) |
|
Colon/rectum |
130,200 (10.7%) |
56,300 (10.2%) |
|
Lymphomas |
62,300 (5.1%) |
27,500 (5.0%) |
|
Bladder |
53,200 (4.4%) |
12,200 (2.2%) |
|
Uterus |
48,900 (4.0%) |
11,100 (2.0%) |
|
Skin (melanoma) |
47,700 (3.9%) |
7,700 (1.4%) |
|
Kidney |
31,200 (2.6%) |
11,900 (2.2%) |
|
Leukemias |
30,800 (2.5%) |
12,100 (2.2%) |
|
Subtotal |
933,000 (76.5%) |
368,800 (66.8%) |
|
All sites |
1,220,100 (100%) |
552,200 (100%) |
|
Source: American Cancer Society, Cancer Facts and Figures�2000. |
||
|
|
||
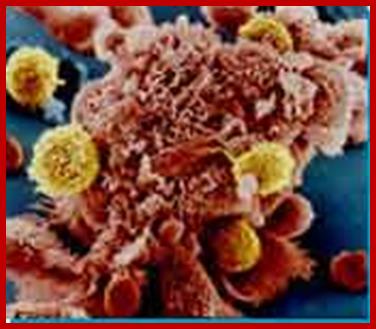 |

Fig: Fully developed cancer in metastasis stage: Melanoma; http://en.wikipedia.org/
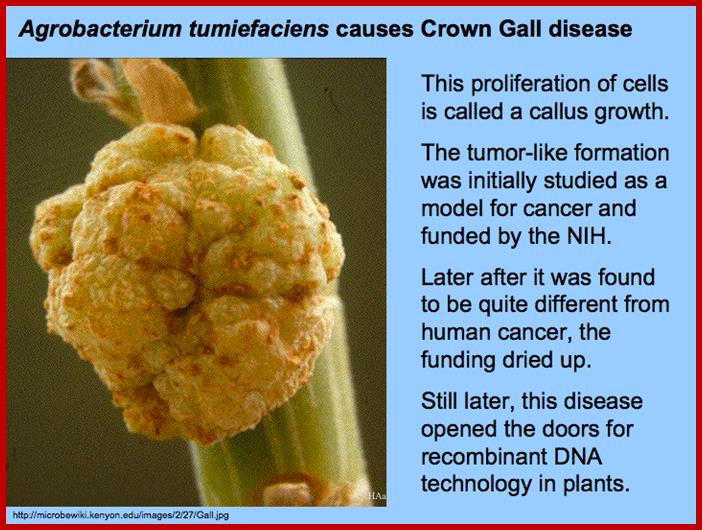
This dreaded disease is not just restricted to humans; it is also prevalent in all organisms, including insects�, unicellular organisms and even in plants.� Depending upon the tissues from which cancer cells are derived they are called Carcinomas and Sarcomas; Carcinomas are derived from ectoderm and endoderm cells and Sarcomas are derived from mesoderm cells. Plants are no exceptions.
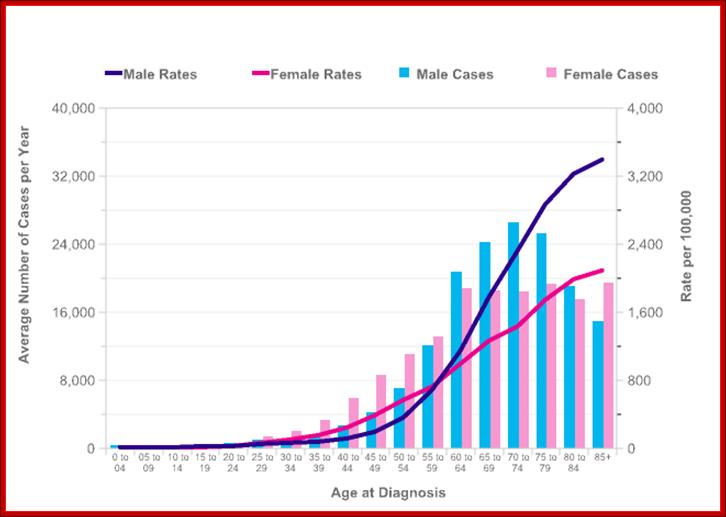
The incidence of cancer depends upon the age factor, indicating cancer is a disease due to accumulation of defects over the time. Statistics of male and females with cancer; �http://www.cancerresearchuk.org/
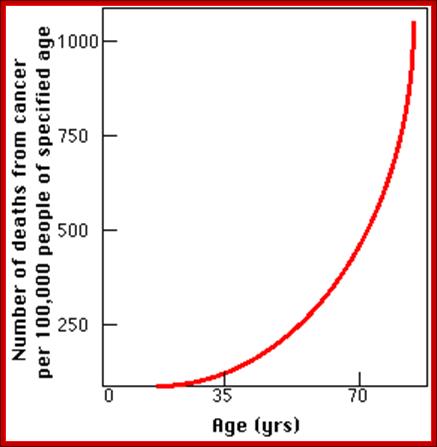
Figure depicts cancer caused death rate to age; http://www.cancerresearchuk.org/
Frequency of occurrence of cancer is to a great extent age dependent; where persons with 40 yr or below has cancer rate is 1.5% of the population, where as persons with 60 yrs or more the frequency increases to 4%, and persons of 80 or above 14%.� This figure also indicates the tissues which have lived such a long period of time, perhaps aged and show senescence of sorts, so their genetic system undergoes changes to make mistakes and go awry.� The aged cells become active and multiply in undifferentiated state and don�t die.
Survey of cancer incidence among the males and females do show some cancers are female specific and some are male specific.� The larger picture of worldwide occurrence can be found that some ethnic groups have high or low incidence.
Do plants get cancer?� Plants are not immune to cancers that produce tumours and galls. Unregulated cell division occurs in plants just like animals, so why don�t we ever hear of a plant dying of cancer?� Agrobacterium tumefaciens causes tumours called crown galls in many species of plant.� The bacteria introduce its own Pi-/Ti DNA into host cells and causes tumour growth can be called Galls.� Ustilago- myadis and Gemini viruses cause tumors in plants.� Do plants die of these cancers???

https://bloomingplants.files.wordpress.com;


http://educatingcreatively.blogspot.in/
A simple survey of cancer among different sexes in humans:
|
Kind of cancer |
Males % |
Females % |
|
Melanoma |
3 |
3 |
|
Oral |
3 |
2 |
|
Lung |
14 |
13 |
|
Breast |
|
32 |
|
Pancreas |
2 |
2 |
|
Colon-rectal |
10 |
12 |
|
Uterus |
|
8 |
|
Ovary |
|
5 |
|
Urinary |
8 |
4 |
|
Prostate |
38 |
|
|
Leukemia |
7 |
6 |
|
Others |
15 |
13 |
|
Cancer site |
Cases per year |
Deaths per year |
|
Breast |
184,200 (15.1%) |
41,200 (7.5%) |
|
Prostate |
180,400 (14.8%) |
31,900 (5.8%) |
|
Lung |
164,100 (13.4%) |
156,900 (28.4%) |
|
Colon/rectum |
130,200 (10.7%) |
56,300 (10.2%) |
|
Lymphomas |
62,300 (5.1%) |
27,500 (5.0%) |
|
Bladder |
53,200 (4.4%) |
12,200 (2.2%) |
|
Uterus |
48,900 (4.0%) |
11,100 (2.0%) |
|
Skin (melanoma) |
47,700 (3.9%) |
7,700 (1.4%) |
|
Kidney |
31,200 (2.6%) |
11,900 (2.2%) |
|
Leukemias |
30,800 (2.5%) |
12,100 (2.2%) |
|
Subtotal |
933,000 (76.5%) |
368,800 (66.8%) |
|
All sites |
1,220,100 (100%) |
552,200 (100%) |
Cancer Gene Census;
|
Sorted By |
Number |
|
Amplification |
15 |
|
Chromosome |
457 |
|
Frame shift mutation |
88 |
|
Germaine mutation |
75 |
|
Large deletions |
34 |
|
Missense mutations |
126 |
|
Nonsense mutations |
85 |
|
Other mutations |
20 |
|
Somatic mutations |
415 |
|
Splicing mutations |
53 |
|
Translocation |
315 |
|
Symbol |
457 |
|
|
|
|
|
|
|
|
|
|
|
|
Incomlete.www.wikipedia.org
Above is the working list of known cancer genes. The list has been
annotated with information concerning chromosomal location, tumor
�types in which mutations are found; classes of mutation that
�contribute to oncogenesis and other genetic disorders mentioned below.
The data has been sorted out in a number of ways to list subsets of cancer
similar features.� However, it is recommended that those wishing to
recommend that those wishing to scrutinize the list in detail and download
�in its entirety.
|
Cancer site |
Cases per year |
Deaths per year |
|
Breast |
184,200 (15.1%) |
41,200 (7.5%) |
|
Prostate |
180,400 (14.8%) |
31,900 (5.8%) |
|
Lung |
164,100 (13.4%) |
156,900 (28.4%) |
|
Colon/rectum |
130,200 (10.7%) |
56,300 (10.2%) |
|
Lymphomas |
62,300 (5.1%) |
27,500 (5.0%) |
|
Bladder |
53,200 (4.4%) |
12,200 (2.2%) |
|
Uterus |
48,900 (4.0%) |
11,100 (2.0%) |
|
Skin (melanoma) |
47,700 (3.9%) |
7,700 (1.4%) |
|
Kidney |
31,200 (2.6%) |
11,900 (2.2%) |
|
Leukemias |
30,800 (2.5%) |
12,100 (2.2%) |
|
Subtotal |
933,000 (76.5%) |
368,800 (66.8%) |
|
All sites |
1,220,100 (100%) |
552,200 (100%) |
|
Source: American Cancer Society, Cancer Facts and Figures�2000. |
||
World wide cancer-141 million-2012; Deaths-8.8 million 2015; Lung (1.69 million deaths),� Liver (788 000 deaths),� Colorectal (774 000 deaths)
Stomach (754 000 deaths),� Breast (571 000 deaths)20165; �http://www.who.int/
Statistics of cancer Incidence among the population of the world (out of 100 000): www.wikipedia.org
High Incidence������������������������������� Low incidence
Lung������������������������������������������������� 110 ���� USA�������������������������������������� 5.8 Madras
Breast������������������������������������������������ 94 ������ Hawaii���������������������������������� 14Israel non-
Jews
Prostate�������������������������������������������� 91 ������ Atlanta��������������������������������� 1.3 China
Cervix����������������������������������� 83 ������ Brazil������������������������������������ 3 Israel n/Js
Stomach������������������������������������������� 82������� Japan������������������������������������� 3.7 Kuwait
Liver�������������������������������������������������� 34 ������ China������������������������ 0.7Canada,
Colon������������������������������������������������ 34 ������ USA�������������������������������������� 1.8 Madras
Melanoma���������������������������������������� 31 ������ Australia-Queensland������ 0.2 Japan Osaka
Nasopharynx����������������������������������� 30 ������ Hong Kong�������������������������� 0.3UK,
Bladder��������������������������������������������� 28 ������ Switzerland Basel�������������� 1.7India �
Ovary������������������������������������������������ 26 ������ New Zealand���������������������� 3.3 Kuwait
Pancreas������������������������������������������� 16�� ������USA
���������� 1.5������ India-Poona
|
Rank |
Country |
Cancer |
|
1 |
Denmark |
338.1 |
|
2 |
France |
324.6 |
|
3 |
Australia |
323.0 |
|
4 |
Belgium |
321.1 |
|
5 |
Norway |
318.3 |
|
6 |
United States |
318.0 |
|
7 |
Ireland |
307.9 |
|
8 |
South Korea |
307.8 |
|
9 |
Netherlands |
304.8 |
|
10 |
Slovenia |
296.3 |
|
11 |
Canada |
295.7 |
|
12 |
New Zealand |
295.0 |
|
13 |
Czech Republic |
293.8 |
|
14 |
Switzerland |
287.0 |
|
15 |
Hungary |
285.4 |
|
16 |
Iceland |
284.3 |
|
17 |
Germany |
283.8 |
|
18 |
Israel |
283.2 |
|
19 |
Luxembourg |
280.3 |
|
20 |
Italy |
278.6 |
|
21 |
Slovakia |
276.9 |
|
22 |
United Kingdom Cancer |
272.9 |
|
23 |
Sweden |
270.0 |
|
24 |
Finland |
256.8 |
|
25 |
Austria |
254.1 |
|
26 |
Spain |
249.0 |
|
27 |
Portugal |
246.2 |
|
28 |
Estonia |
242.8 |
|
29 |
Poland |
229.6 |
|
30 |
Japan |
217.1 |
|
31 |
Turkey |
205.1 |
|
32 |
Chile |
175.7 |
|
33 |
Greece |
163.0 |
|
34 |
Mexico |
131.5 |
�
*List of OECD countries and their cancer rate; new cancer rate based on 100,000 populations.
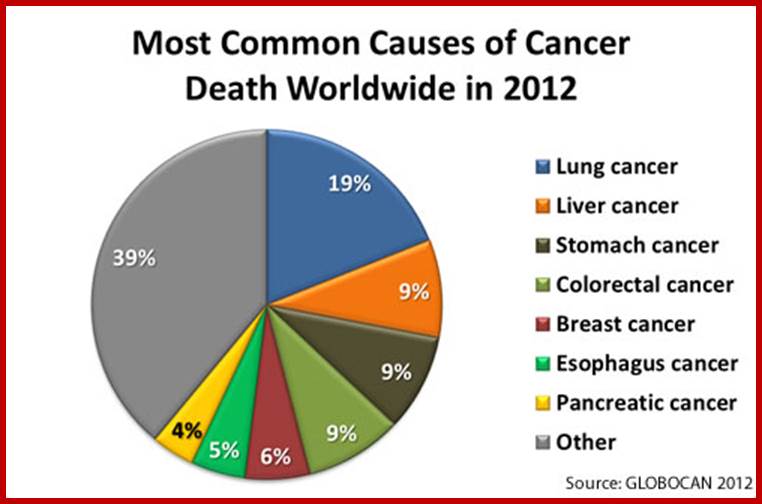
Death due to cancer worldwide (2012)
� Lung (1.59 million deaths)
� Liver (745 000 deaths)
� Stomach (723 000 deaths)
� Colorectal (694 000 deaths)
� Breast (521 000 deaths)
� Oesophageal cancer (400 000 deaths) (1).
Note-14.1 million diagnosed with cancer, 8 million died. And 21.7 million are expected to be with cancer by 2030 and 13 million deaths expected due to cancer Epidemiology and End Results [SEER] Program)- the Centers for Disease Control and Prevention (National Program of Cancer Registries), and the North American Association of Central Cancer Registries. �Mortality data were collected by the National Center for Health Statistics. In 2016, 1,685,210 new cancer cases and 595,690 cancer deaths are projected to occur in the United States. Estimated new cases-841,390, estimated deaths-314290-in USA https://www.ncbi.nlm.nih.gov
Cancer Genes and Their Numbers:
The total number of genes involved in inducing or causing cancer is statistically surveyed, and they are found to be 291 to 321; this estimate has come from several sources including Sanger�s institute of science and from an article published by a group of scientists in the journal -Nature.
Estimated number of genes involved in cancer including functional categories:
Total number of human genes identified and characterized is ~350
(From Sanger�s institute of cancer), of which 311 have one or the other
Kind of mutations in somatic cells; this account for all Human cancer
�types known. This is an ongoing survey and the results are
Published periodically and updated with time.� Scientists in Cancer genome
Project have identified and classified them accordingly.
- A survey of different types of cancers and the number of identified as
- �cancer-causing genes is about 291genes and
311 to 320 (2016) (Nature 2004 Mr. Stratton) accounts for 1% of human
�genes. According to International Cancer Genome Consortium ICGC
may, 16 2016 the Number of cancer-causing genes is ~81
- Nearly 1% of the human genes are involved.
- Of which 70-90% of them are due to somatic mutations, 20% due to
germ line mutations, and 10% are due to both.�
- Most of them are due to chromosomal translocations.
- More number of cancer genes has been found in leukemia, lymphomas and sarcomas than in any other types of cancer cells, yet they represent 10% of all the cancer genes (mostly due to translocations0).
- The most common cancer-causing proteins are found to contain kinase domains, DNA binding domains including transcriptional regulators i.e. transcriptional activators and suppressors.
- Transcriptional and regulatory factors account for 26.7%, Structural changes 11.2%, Phophorylation-kinases and their inhibitors account for 16.2%, DNA repair dysfunctions �9.6%, defects in Ubiquitination �1.8%, others and unknown account for 24.3%.
- In some miRNA genes are also involved.
- Cancer genes also carry several passenger or bystander mutations.
Features of Normal Cells under Culture Conditions:
� Normal and healthy cells in cultures divide and redivide, but stop after reaching certain number of divisions, which is called Hayflick limit and perhaps end up in crisis.
- Cells require serum for it provides stimulus in the form of growth factors.
- Cells grow in monolayers.
- Cells show contact inhibition and adhere to the substrate for they have binding and interacting extra cellular matrix.
- They retain cell shape of their progenitors.
Immortalization:
When cells are grown under in vitro culture, cells go through 10 or more cycles of cell division, the go through crisis.� Human cells can go through 40 cycles of division before death.� Few cells come out of the crisis and rest of them die.� With repeated cell divisions and aging, telomeres are lost; this can lead to crisis because of lack of Telomerase.� Often such cells suddenly acquire Telomerase activity and continue to divide and redivides, this is in spite of having genetic defects especially chromosomal abnormalities, and establish non-tumorigenic cell lines.� They are considered to be immortalized cells; such cells have all the potentiality to develop into cancer cells.� Such immortalized cells have few distinct features of their own.
� They look like their progenitor cells.
� They require solid surface for their proliferation similar to that of normal cells.
� Require some amount of serum.
� The growth will be inhibited at a particular density.
Cells have elongated network of cytoskeleton especially microfilaments called stress fibers.� Most of these cell cells have suffered chromosomal damages in one-way or the other, or gene mutations of one type or the other. �
Important Features of Cancer Cells:
- Cells are the survivors of the crisis. They have acquired new genetic mechanism tide over all the control mechanisms.
- Development of cancer is a multistep process in which cells gradually become malignant through progressive alteration.
- First step in the process is thought to be the result of genetic alterations leading to abnormal proliferation and then leads to outgrowth of population
- They show transformed morphology, mostly spherical shape.
- Many cancer cells fail to undergo Apoptosis, loss of contact inhibition and loss of density dependent contact inhibition.
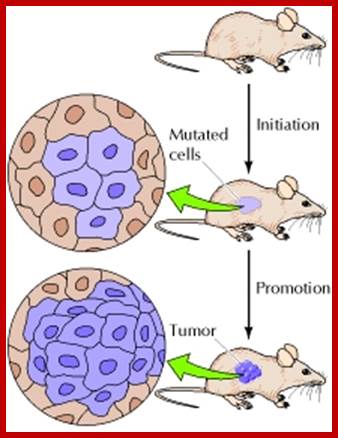
Induction of tumor in mouse skin. http://www.ncbi.nlm.nih.gov/

Density-dependent inhibition: Normal cells proliferate in culture until they reach a finite cell density, at which point they become quiescent. Tumor cells, however, continue to proliferate independent of cell density. http://www.ncbi.nlm.nih.gov/
The leukemia provides a good example of the relationship between defective differentiation and malignancy. �Develop from stem cells in the bone marrow.
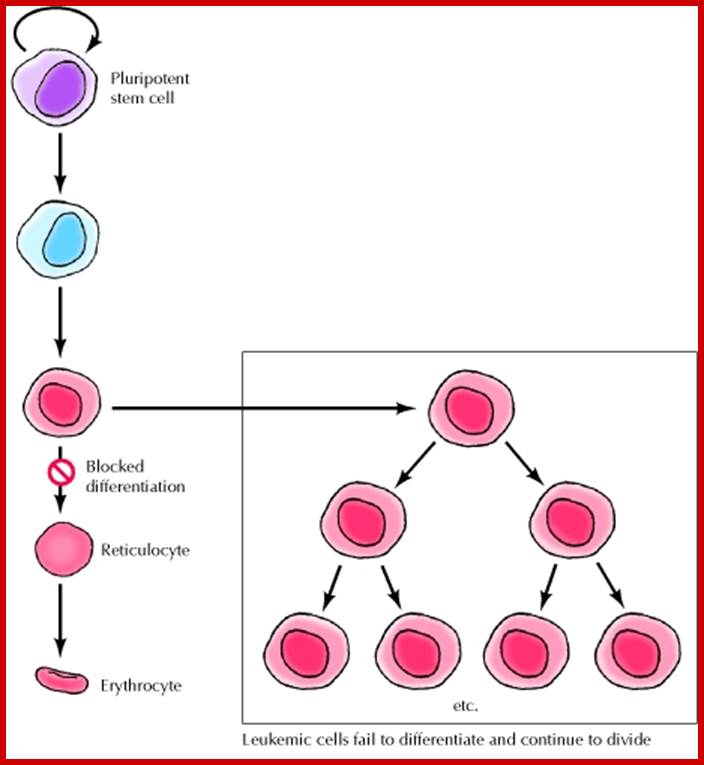
Defective differentiation and leukemia; ncbi.nlm.i.nhi.gov

Kidney cancer;� http://www.robertsreview.com/
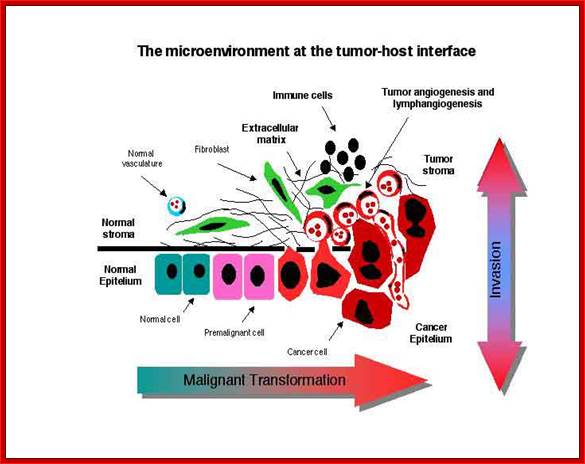
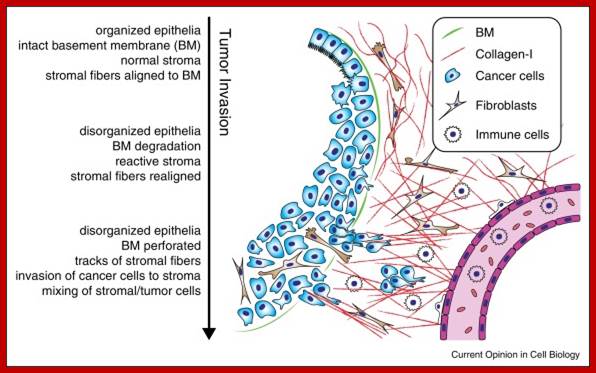
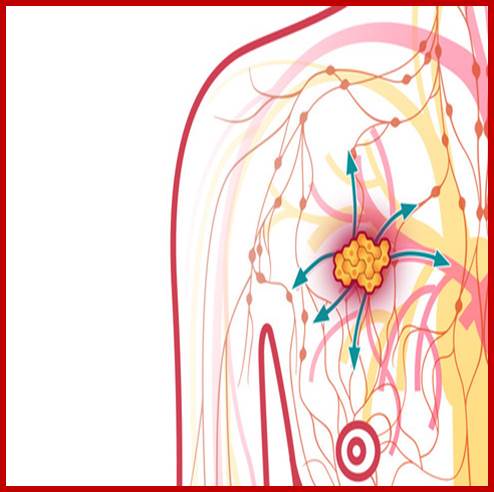
Cancer cells invading its neighboring cells and tissues; Andrew G Clark and��
� Danijela Matic Vignjevic http://www.sciencedirect.com
- They grow independent of serum in vitro.� Can they grow without nutrition?
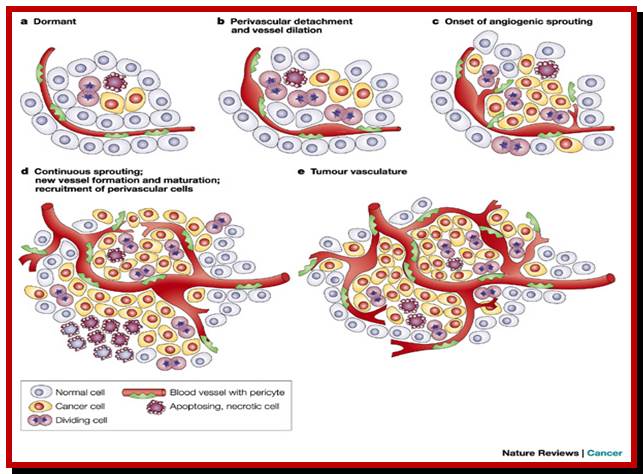
- They have sustained angiogenesis for they produce their own growth factors for the growth of blood vessels, ex. bFGF, VEGF (vascular endothelial GFs) and TGFs (transforming GFs).� They have developed autocrine system.
- Insensitive to antigrowth factors.
- They have lost extra cellular matrix and cell adhesion and basal lamina; thus, they have lost contact inhibition.
- Cells produce and release plasminogen activator that converts serum plasminogen into an active plasminogen protease thus digestion of extra cellular matrix is lost.
- They invade the underlying connective tissues.
- A single cell initially altered gives rise to proliferative cell population.
- They generate their own cell surface proteins; thus, they evade immune surveillance.
- Lost senescence and apoptotic properties.
- They have internal microfilaments reorganized
- They pile up and produce foci.
- They show no contact inhibition for their extra cellular matrix is deformed.
- They have reorganized intracellular microfilaments thus they show changed morphology.
- They can divide and redivide forever and migrate from one site to the other.
- They have an extraordinary and limitless replication potential and cell cycle regulation has gone haywire.
- They show high metabolic activity, with large Nucleus and large nucleolus.
- The DNA from cancers cells can easily transform other cells into cancer cells.
- Cells proliferate but not differentiate.
- Carcinomas, approximately 90% of the human cancers, they are the malignancies of epithelial cells.� Sarcomas are solid tumors of connective tissues.
- The four most common cancers, accounting for more than half of all cancer cases, are those of the breast, prostate, lung, and colon/rectum.
- Lung cancer, by far the most lethal, is responsible for nearly 30% of all cancer deaths.
![]()
http://www.ncbi.nlm.nih.gov/Tumor clonality
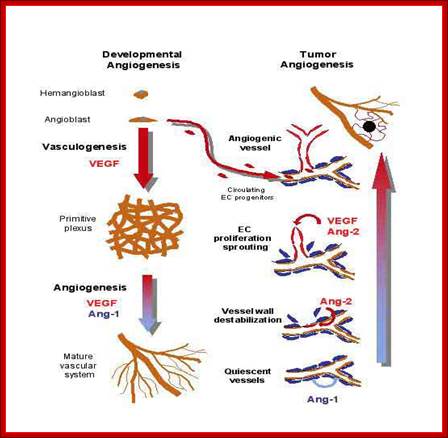
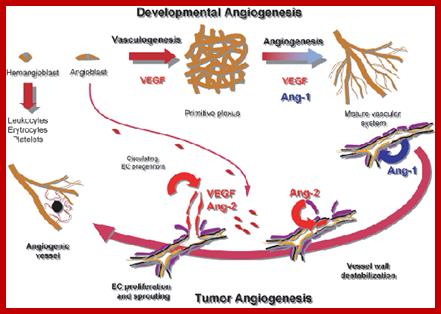
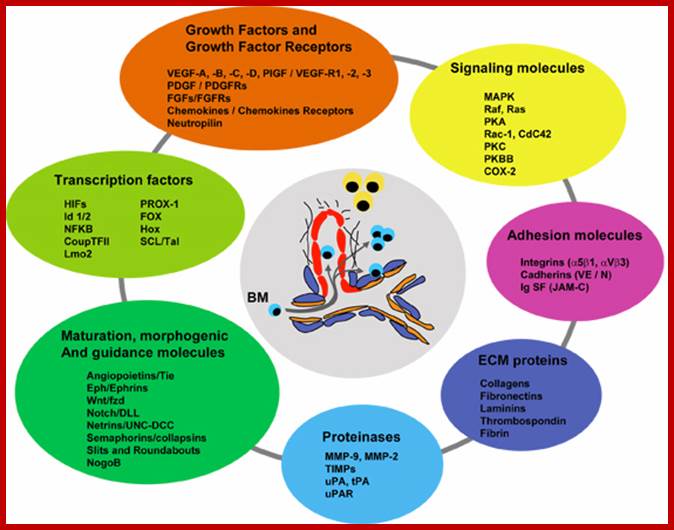
Angeogenesis and tumor angiogenesis; http://www.unifr.ch
http://www.healthline.com/
����������� Figures show growth of blood vessels into tumors; http://slideplayer.com/
����������������������������������� ����������� 
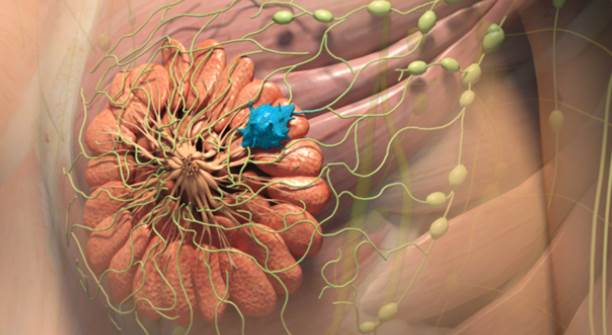
Spread of cancer cells via vascular system. ��������http://www.wallstreetotc.com/breast-cancer-tumors
Stages of cancer development;; https://science.education.nih.gov
![]()
The classical angiogenic switch. http://www.nature.com/
����������� ����������������������� �� �
The central role of DNA damage and epigenetic defects in DNA repair genes in carcinogenesis; https://en.wikipedia.org/wiki/
When normal cells are damaged beyond repair, they are eliminated byapoptosis (A). Cancer cells avoid apoptosis and continue to multiply in an unregulated manner(B).; https://en.wikipedia.org/wiki/
Cancers are not due to single gene defect:
Cancer can be due to many factors, such as carcinogens, age, persons genetic stability, persons immune system, diet, environment and it can be due to different types of viruses.� Cancers are due to combined action of many genes, some time the number can be 50 or more, but the combination of changed genes has profound effect on the cancer development. The full blown-up cancer takes over a period of time with a series of mutation of genes and a combination of defective genes with a course of time.
Adenomatous polyposis coli:
Adenomatous polyposis coli, it is a colon cancer.� How this cancer is developed stepwisely is described below.�

Just to show the size;
impact of cancer-young and old
This is just a pictorial showing the enormity of cancer development from a small sized tissue.
- It starts with a mutation in APC gene (chromosome 5), not necessarily it should be APC gene.� The APC gene products are responsible for the repairing damaged DNA , actually it is a tumor suppressor gene. �APC gene is involved in Wnt �β-catenin induced transcription of� Myc gene.
- Mutation or damage to APC-DNA is not repaired and this mutation leads to the development of polyps in the colon. APC gene product is involved in Wnt. pathway.� Among many members of complex of proteins that act in Wnt induced signaling pathway, APC is one of them.� APC is associated with other protein as a complex of proteins; they are- b-Catenin, Axin/Conductin GSK-3b.� Among them GSK-3b is a phosphorylating enzyme; this is actually a kind of scaffolding complex.� In the absence of Wnt signal, APC binds to beta Catenin and the associated kinases phosphorylate b-catenin, which then ubiquitinated and degraded by Proteosomes.� In the absence of functional APC, the b-Catenin protein gets stabilized and it enters the nucleus where in association with TCF factors activate the expression of Myc gene, which favors G1-S pathway.� Believe it or not b-catenin is also the protein that binds to C-adherins at extracellular space involved in cell to cell adhesion.
- So absence of APC favors the Myc expression that leads to overcome G1-S checkpoint.
- Further progress of colon cancer depends on mutation of RAS genes (chromosome 12).
- Loss of check points from G1 to S, G2 to M and metaphase to cytokinesis via anaphase.
- Loss of P53 (tumor suppressor) chromosome 17, allows and aggravates progress towards uncontrolled cell division.
- Loss of Pro-apoptotic genes.
- Loss of antiproliferation factors like TGF-b.
- Accumulation several more defects over a period of time, there can be more than 5-75 changes.
- All these lead to fully-blown colon cancer from a tiny cell..
To illustrate the point, scientists have created transgenic mice with over expressing genes such as Myc and Ras.� With Myc gene, alone over expressing, �in about 100 mice, over a period of hundred days, few mice get cancer.� In mice over expression of Ras, in about hundred mice over a 100-day period about 50 mice get cancer.� But with both Myc and Ras genes expressed in the same mice, all hundred mice get cancer in 50 days time.� This experiment demonstrates the deadly combination genes make cancer develop quickly.� Ras DNA alone, cultured cells can cause cell transformation that is the deadliest effect the RAS can produce. Majority of the cancers suffer loss of G1-S, G2-M and M-cytokinesis checkpoints.� In another situation when Myc is expressed it remains for a long duration in the cells, but when fos is expressed, it half life is short and gets degraded.� If the expression and the stability of fos is sustained for a longer period, then cell transformation is possible for both and Myc and Fos are transcriptional factors.
Some common cancers:
Oral, Bladder, Bone, Brain, CNS, Breast, Cervical, Colon, Gastric, Hodkins lymphoma, Kidney, Leukemia, Lung small cell, Lung non-small cell, Lung, Melanoma, Mesothelioma, Multiple myeloma, Myelodysplastic syndrome, Non-Hodkins lymphoma, Ovarian, Pancreatic, Prostate, Rectal, Renal, Skin, Testicular, Throat, Thyroid, Uterine cancer and others. For that matter all cell types located in various types of tissues can be potentiated to develop into a cancer tissue only in stepwise manner.
�Human body consists of at least 320 or so cell types, for any of the cell types can develop cancer that does not mean there are 320 different types of cancer-causing genes.� Even one cell type to develop into transformed and cancerous type, action of many genes are required; and often a combination of them.� ���
The names of genes responsible were named on the basis of organ or tissues from which they were identified for the first time.� Many a times the names assigned may be due to other reasons.
Killer T cells (ornage) are recruited to attack malignant cells in the viral (Herpes) based therapy-T-VEC; This Picture depicts the full blown cancer tissue in metastasis stage; Heide Ledford http://www.nature.com/
�����������������������������������������������������������
��������� Ten most common types of cancers:
�Esophageal cancer; Ovarian cancer; Liver and Intrahepatic bile duct cancer; Non-Hodgkin lymphoma; Leukemia; Prostate cancer; Pancreatic cancer; Breast cancer; Colon and rectal cancer; Lung and bronchial cancer; Lung cancer; Bladder cancer; Kidney cancer; Skin cancer; Melanoma; Thyroid cancer; Pancreatic cancer; Cervical cancer; stomach cancer; Prostate cancer.
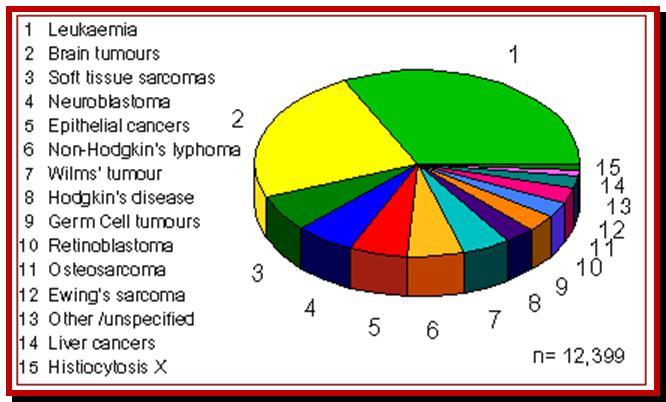
Different cancers in childhood based on UK data from The National Registry of Childhood Tumours ; http://www.cancerindex.org/
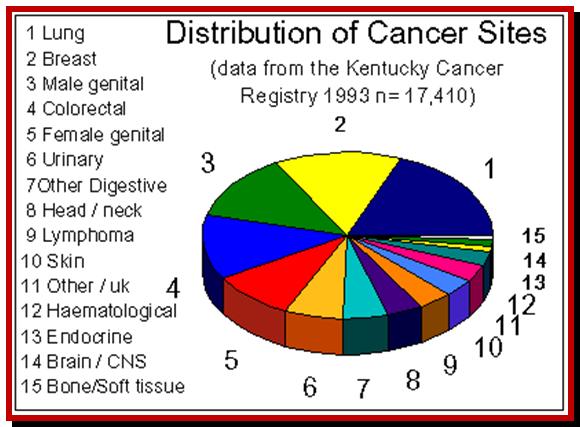
Adult cancers; http://www.cancerindex.org/
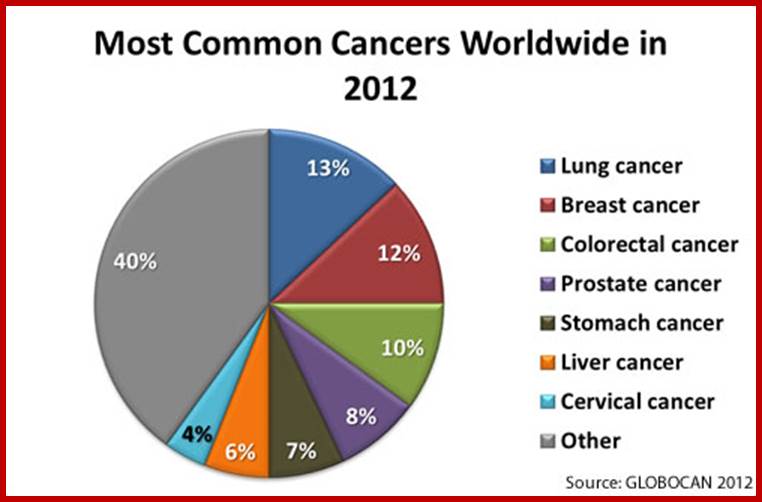
Global cancer statistics-2012; http://www.cdc.gov/
http://www.cdc.gov/cancer/international/statistics.htm
In 2012, the most common causes of cancer death worldwide (for both sexes) were*�
1. Lung cancer (19% of all cancer deaths; 1.6 million people).
2. Liver cancer (9% of all cancer deaths; 745,000 people).
3. Stomach cancer (9% of all cancer deaths; 723,000 people).
4. Colorectal cancer (9% of all cancer deaths; 694,000 people).
5. Breast cancer (6% of all cancer deaths; 522,000 people).
6. Cancer of the esophagus (5% of all cancers diagnosed; 400,000 people).
7. Pancreas cancer (4% of all cancers diagnosed; 330,000 people).
Breast cancer; http://www.med.helsinki.fi/; https://www.google.co.in

Skin cancer; Klaus Wolff, Richard Allen Johnson, Dick Suurmond; http://www.medicinenet.com/
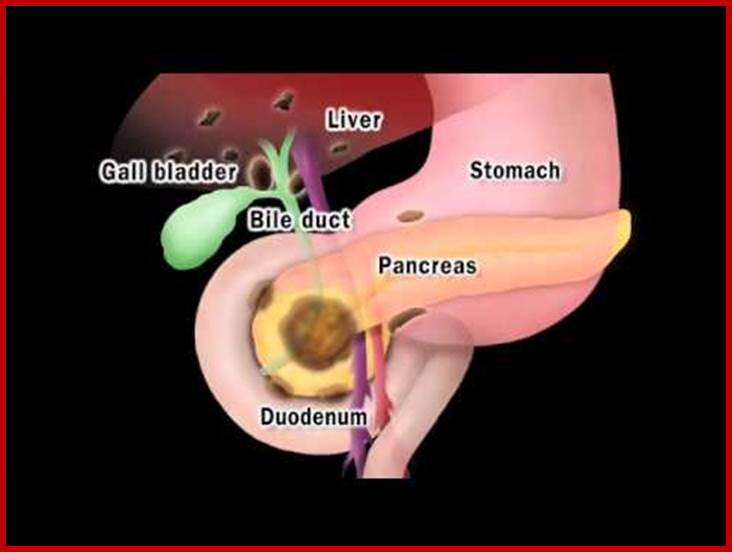
Pancreatic Cancer; www.Utube.com

Lung cancer;www.bionews-tx.com

Human colon cancer; http://acceleratingscience.com/
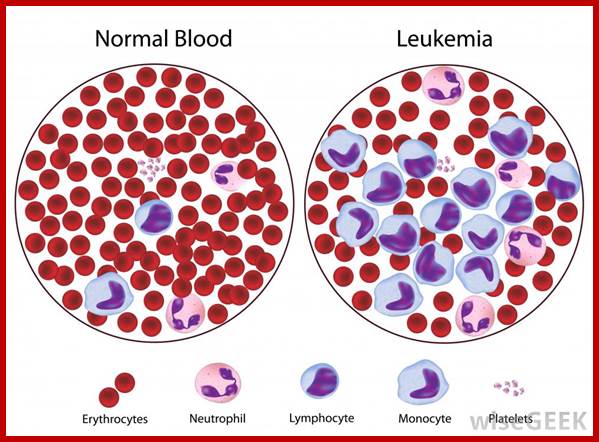
Blood from halthy person and one with leukemia showing� increase in hye number of WBC; http://www.wisegeek.org/
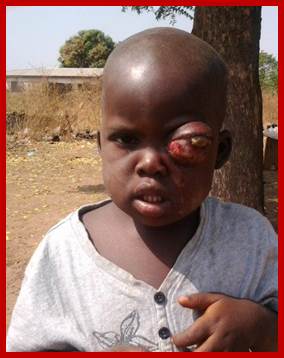
 �http://wechope.org/retinoblastoma;
http://vrachfree.ru/en/diseases-en/
�http://wechope.org/retinoblastoma;
http://vrachfree.ru/en/diseases-en/
Some of the Cancer genes and Cancers:
v-abl�������������� Abelson murine leukemia,
APC��������������� Adenomatous polyposis coli.
Bcl1.2� ����������� B-cell lymphoma,
Bcr����������������� Break point cluster,
Braf���������������� v-raf murine sarcoma,
Crk���������������� v-crk avian sarcoma,
ErbA�������������� v-erb2 erythroblastic leukemia,
Fes����������������� feline sarcoma,
Fos����������������� v-fos FBJ murine osteosarcoma,
Hras�������������� V-Hras Harvey rat sarcoma,
Jun����������������� v-jun avian sarcoma,
Kras��������������� V-Ras Kirsten rat sarcaoma,
MEN1 Multiple endocrine neoplasis,
Mos��������������� V-mos Moloney murine sarcoma,
Myb��������������� v-myb avian myeloblastasis ,
Myc��������������� v-myc Avian Myelocytomatosis,
Nras�������������� v-ras neuroblastoma,
RB������������������ retinoblastoma,
Rel����������������� v-rel Avian reticuloendotheliosis,
SpII���������������� v-spII spleen focus farming oncogene,
Src����������������� v-src rous avian sarcoma,
Tp53�������������� Li-Fraumeni syndrome,
WT1��������������� Wilms tumor,
Yes����������������� v-yes Yamaguchi sarcoma.
The above list is only few. But the list shows 571 cancer causing genes; Mutations in at least 291 human genes are casually implicated in oncogenesis, and all of them encode protein coding genes, but none of them have been identified to produce sn RNAs.� Nearly 90% of cancer causing genes show somatic mutations and 20% show germline mutations. http:// cancer.sangers.ac.uk/census/
A distinction should be made to understand terms such as C-oncogenes means proto-oncogenes.� C-oncogenes are the oncogenes mutated from the normal cellular genes.� V-oncogenes means retroviruses in their life cycle occasionally pick cellular genes and when they reinfect, the cellular gene modified or normal, is over expressed because the expression of such genes are the under the control of retroviral enhancer elements.� Some such genes, identified are called V-oncogenes and most of them have suffered one more mutation or deletion.� Proto-oncogenes are the cellular genes have the potentiality to develop into oncogene if they suffer mutation or placed in a site for over expression.�
There are many viral- DNA encoded genes whose products, most of the times, bind to tumors suppressor genes and facilitate the development of cancer, they are the true Viral-Oncogenes.
APC
This tumor suppressor gene is named for a condition with which it is associated � familial adenomatous polyposis coli, a viciously premalignant disease with thousands of polyps contributing to inherited colorectal cancer in certain untreated gene carriers.
BRCA1
Mutations in this tumor suppressor gene, which encodes breast cancer type 1 susceptibility protein, are thought to be responsible for nearly half (45 percent) of inherited breast cancer (five percent of all breast cancer) cases and more than four in five cases of inherited breast and ovarian cancer.
A positive family history for breast cancer, which affects one in eight women during their lifetime, has been identified as major contributor to risk of development of the disease. This link is particularly striking for early- onset breast cancer.
BRCA1 mutation carriers are also four times as likely to develop colon cancer as their non-carrier counterparts; male carriers face a three-fold increased risk of prostate cancer.
BRCA2
This gene codes for a protein believed to play a role in the repair of DNA and/or exchange of DNA during cell division, or homologous recombination.
Believed to be responsible for some inherited breast cancer in women, BRCA2 is also linked with male breast cancer.
CDK4
Research suggests that cyclin-dependent kinase 4, the protein encoded by the CDK4 gene, is involved in regulating the natural circadian rhythm of cells (cell cycle). Mutations in this gene have been shown to be involved in formation of certain non-hereditary cancers.
CMM1
Mutations in the CMM1 gene are associated with familial malignant cutaneous melanoma.
HER2
Also referred to as NEU or ERBB2, this gene encodes for a protein which is essential component of a complex of molecules on the surface of cells called the neuregulin-receptor complex.
Associated with non-hereditary breast cancer, HER2 made headlines when biotechnology giant Genentechreleased its anti-cancer drug, Herceptin, which is used to treat patients whose breast tumors display an excess of HER2 protein.
MLH1
Believed to play a role in fixing erroneous DNA replication, the MLH1 gene is associated with familial hereditary nonpolyposis colon cancer (HNPCC). HNPCC is one of the most common genetic diseases in the western world, accounting for up to ten percent of all colon cancers.
MSH2
Named for a mutation first discovered in the bacterial counterpart of the human gene, the MSH2 gene is associated with a hereditary form of colon cancer (hereditary nonpolyposis colorectal cancer, HNPCC), which accounts for up to one in ten cases of the disease.
Alterations in the MSH2 and MLH1 genes are the most common mutations in families with multiple cases of HNPCC � together, they account for over 90 percent of mutations found in these individuals.
Like MLH1, the MSH2 protein is also involved in repairing errors during DNA replication.
p16
Also called CDKN2, protein 16 has been shown to slow the growth and division of normal cells. Errors in the gene, presumably resulting in unbridled growth and division, are involved in tumor formation in a wide range of tissues, including skin (resulting in melanoma).
p53
Normal protein 53 suppresses the development of many tumor types. It has been shown that to do so in a number of ways, including arresting the growth or even actually programming cells to die, depending on the physiological circumstances or cell type.
The protein is mutated or inactivated in about 60 percent of cancer cases; it is found in increased amounts in a wide variety of transformed cells.
For instance, variants in p53 cause a familial cancer syndrome called Li-fraumeni syndrome; in these families, the affected relatives develop a diverse set of malignancies including leukemia, breast carcinomas, sarcomas (bone tumours), and brain tumours at unusually early ages.
p53 mutations are also the cause of Barrett�s adenocarcinomas, a disease of the lower oesophagus which develops as a complication in about one in ten patients with chronic untreated heartburn (gastroesophageal reflux disease).
Defects in p53 cause additional cancers, including head and neck squamous carcinomas.
Rb1
One of the most important examples of a gene associated with hereditary cancer, Rb1 was used to describe the �two-hit theory� for hereditary cancers, which holds that in individuals carrying predisposing germ line mutations, cancer may occur as a result of an additional, non-inherited mutation.
Deletion or alteration of this protein results in the childhood eye cancer- retinoblastoma. This disease represents about two percent of all childhood malignancies
Although most cases of retinoblastoma appear sporadically, about one in five is transmitted as a genetic trait which may or may not show clinical symptoms. The Rb1 protein is believed to regulate the expression of other genes, acting as a tumor suppressor. Refer to http://www.eupedia.com/genetics- http://www.geneletter.com/
Carcinogens:
Any factor that is capable of inducing uninhibited mitosis� that lead to the production of mass of cells called cancer, is called carcinogenic agent; it can be an environmental factor, a chemical or radiations, which damage DNA, enzymes �and its coding information and enzymes to be abnormal. �The number is a long list, only few of them are listed.
Acroliens,
Allylthiocyanate,
p-aminoazobenzene,
Asbestos,
Azacytidine,
Benzaanthracene,
Benzene based dyes,
Benzo pyrene,
Bleomycins,
Carbon-black,
Ceramic fibers,
p-chloroaniline,
Chromium,
Cisplatin,
Coal-tars,
1,4 chlohexadienes,
DDT 9dichloro diphenyl dichloro ethylene),
p-dichlorobenzene,
Ethylmethae sulfonate,
Ethylene di bromide,
Ethylene urea,
Heptachlo epoxide,
Lead phosphate,
Methylazoxymethanolacetate,
Methyl cholanthrene,
N-methyl nitrosourea,
Nickel compounds,
Nitroflurazones,
Nitrogen mustard n-oxide,
N-nitroso n ethyl urea,
Phenoxybenzamine hydrochloride,
Radionuclides,
Rhodamine,
Saccharins,
Thorium dioxides,
Uracil mustard,
Urethane,
X-rays,
Gamma rays,
Potent free radicals,
Hydroxyl radicals.
http://monographs.iarc.fr/and https://en.wikipedia.org/wiki/List_of_IARC_Group_1_carcinogens;
Cancer cells acquire self-sufficiency in its growth, loss of sensitivity to antigrowth signals, loss of capacity to apaptise, loss of senescence, acquire sustained angiogenesis, capable of invading into neighboring tissues, they acquire ability for metastasis, control in the numbers they produce, they also acquire and cause mutations.
Cancer cells develop Self immunity:
The widespread T cell recognition of self-antigens on human cancer cells is surprising. Insights into the relevance of T cell recognition of non-mutated self-antigens have stemmed from studies of spontaneous tumors in mice. These tumors are weakly immunogenic, yet arguably are more representative of most human cancers than the strongly immunogenic mutagen-induced tumors. http://www.ncbi.nlm.nih.gov/
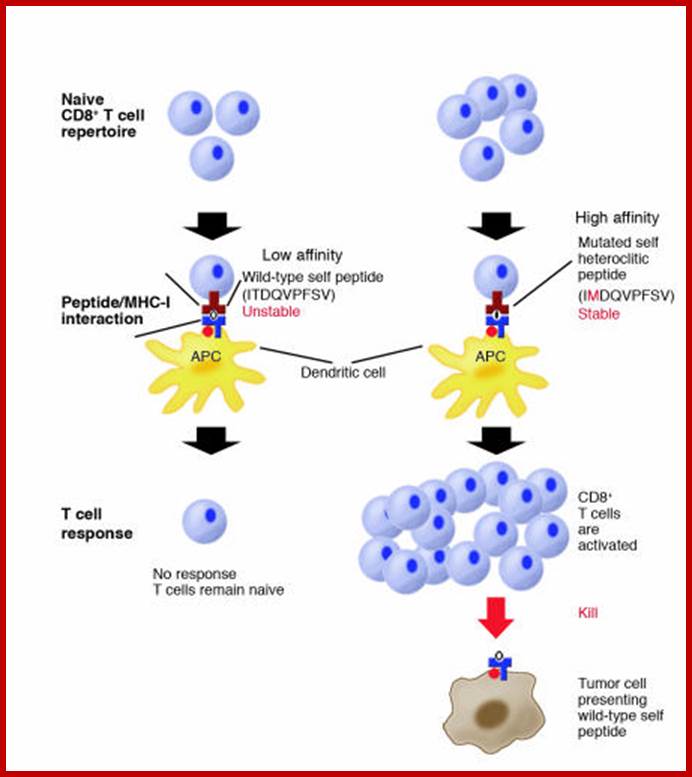
Yu et al. (16) investigate how host CD8+ T cells respond to a self-peptide presented by MHC-I molecules on tumor cells. The self-peptide binds relatively weakly to host MHC molecules. The self-peptide, �ITDQVPFSV (single letter amino acid code), expressed by melanoma cells and normal pigment cells, binds with low affinity to MHC-I HLA-A*0201 molecules. A mutated form of the self-peptide, IMDQVPFSV with a threonine to methionine substitution at the second amino acid position, has a high affinity for MHC-I molecules because methionine residues at the second position are more favorable to anchor the peptide to HLA-A*0201 molecules. Naive CD8+ T cells against the self-peptide are present in the immune repertoire, but they do not respond to either tumor cells presenting the weak self-peptide or to immunization with the self-peptide because of the instability of self-peptide/MHC complex. However, immunization with the mutant self-peptide activates the host T cells. The mutant peptide is presented by MHC-I molecules on dendritic cells, which are potent APCs. Once the CD8+ T cells are activated, they are competent to recognize and kill host tumor cells presenting the nonmutated self-peptide. These results show that T cells recognizing a self-antigen are capable of killing tumor cells presenting the self-antigen following activation with the mutated form of the antigen. www.NIH.NCB.org.
Suggested mechanisms of origin for tumor antigens include;
� Introduction of new genetic information from a virus (eg, human papillomavirus E6 and E7 proteins in cervical cancer)
� Alteration of oncogenes or tumor suppressor genes by carcinogens, which result in formation of neo-antigens (novel protein sequences or accumulation of proteins that are normally not expressed or are expressed at very low levels, such as ras or p53 ), either by generating the novel protein sequence directly or by inducing accumulation of these proteins
� Missense mutations in various genes not directly associated with tumor suppressor or oncogenes and that cause appearance of tumor-specific neo-antigens on the cell surface
� Abnormally high levels of proteins that normally are present at substantially lower levels (eg, prostate-specific antigens, melanoma-associated antigens) or that are expressed only during embryonic development (carcino-embryonic antigens)
� Uncovering of antigens normally buried in the cell membrane because of defective membrane homeostasis in tumor cells
� Release of antigens normally sequestered within the cell or its organelles when tumor cells die
- The development of cancer and autoimmunity can be seen as a failure of the immune system to control tumour cell growth and to regulate auto reactive responses, respectively. The immune system is finely balanced to distinguish foreign from self-antigens.
- Normally, peripheral tolerance keeps potentially auto reactive lymphocytes in check because recirculating lymphocytes are exposed to tissue antigens under non-inflammatory conditions, which results in a tolerant, anergic state. http://www.ncbi.nlm.nih.gov/, http://www.ncbi.nlm.nih.gov/, http://www.ncbi.nlm.nih.gov/
Autoimmune disease: �Prominent examples include celiac disease, diabetes mellitus type 1, sarcoidosis, systemic lupus erythematosus (SLE), Sj�gren's syndrome, Churg-Strauss syndrome, Hashimoto's thyroiditis, Graves' disease,idiopathic thrombocytopenic purpura, Addison's disease, rheumatoid arthritis (RA), ankylosing spondylitis, polymyositis (PM), and dermatomyositis (DM). It is an accepted fact that autoimmune responses are an integral part of vertebrate immune systems (sometimes termed "natural autoimmunity"), normally prevented from causing disease by the phenomenon of immunological tolerance to self-antigens. https://en.wikipedia.org.
�����������������������������������������������